How is cataract surgery performed?
Cataract surgery is one of the most frequently performed operations worldwide. There have been so many advances that have made this procedure more safe and effective than ever.
Typically, cataract surgery is performed with the patient lying down on an operating table under local anaesthetic, however general anaesthetic can be used. General anaesthetic is usually required for conditions such as Parkinson’s disease where it may not be possible to keep for the duration of the procedure. Anxiety or claustrophobia is another reason for using general anaesthetic. Local anaesthetic can be combined, if required, with a mild anxiolytic such as Diazepam or Temazepam, which can help make the whole experience less stressful.
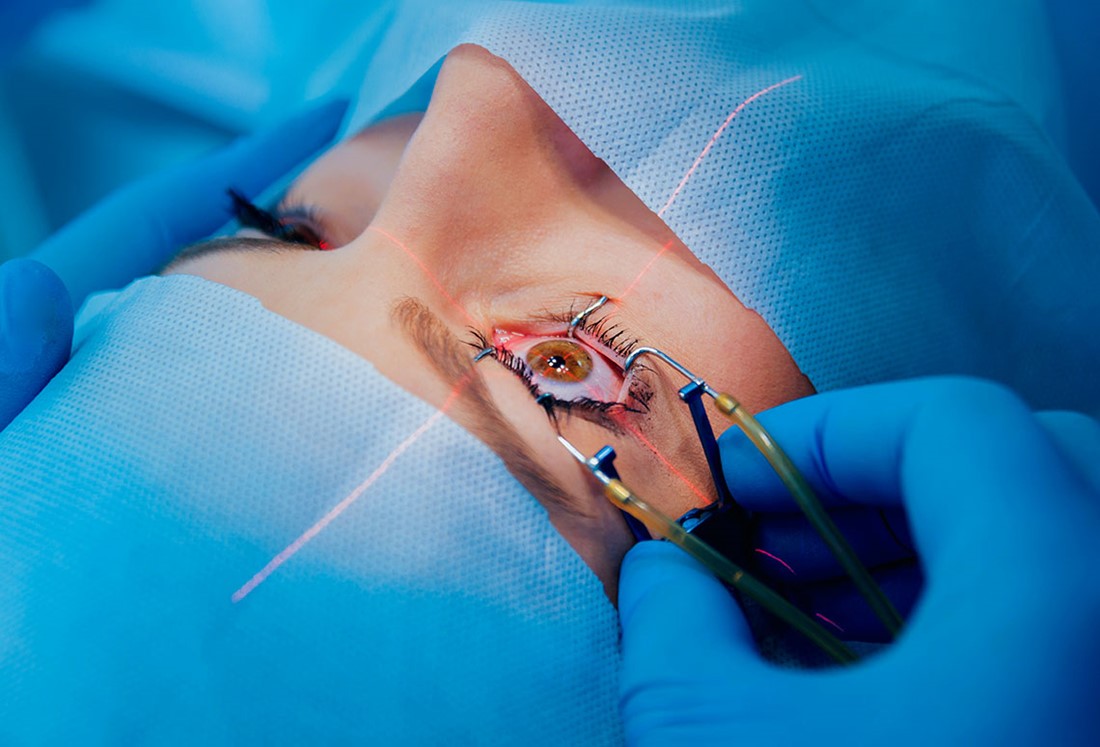
Prior to surgery, numbing drops and iodine will be put in the eye. This is a vital step to prevent postoperative infection. The eye and face will be cover with sterile blue sheets and a speculum is used to hold the lids open, which will prevent blinking. Mr Modi typically will use a sub-tenons anaesthetic which means that the eye will not move and also it will not be possible to see anything during the procedure out of the eye as the optic nerve is also numbed.
A microscope is used, which has a very bright light. It is operated with a foot pedal, which helps focus, magnification, position and adjusts the brightness of the light.
To start, two small incisions are made in the cornea at the front of the eye. These are both between around 1-2 mm in width. The surgery is performed through these incisions and as such it can be thought of as a type of ‘micro-laparoscopic’ surgery. The eye remains formed as a jelly-like substance called viscoelastic is used to fill the eye and keep its shape during the next steps.
The lens itself is wrapped in a layer called the capsule, which is thin and transparent, a bit like cling-film. A round opening is made in this capsule measuring around 5 mm in diameter. The phacoemulsification probe, a bit like a large pen, is placed inside the eye through the larger incision. This breaks up the lens using ultrasound energy. The probe has an opening in the centre that aspirates the broken-up lens material.
Once the capsular bag is empty, the new lens, made of acrylic plastic is placed inside the bag. This lens is selected based on measurements or ‘biometry,’ performed prior to surgery. It goes in folded and slowly unfolds like a ‘ship in a bottle.’ The lens that goes into the eye, if surgery is uncomplicated, will remain in place for life and should never need to be replaced.
Antibiotics are given inside the eye to prevent infection. Cefuroxime is currently favoured however is avoided in cases of cefuroxime anaphylaxis. The small incisions are ‘hydrated,’ which helps them self-seal. Occasionally a suture is placed if needed and this can be removed in clinic over the following weeks.
An eye shield is placed over the eye to protect it and this will remain in place until the next morning. Advice is given to wear the clear eye shield over night for the first week by taping it over the eye. Following surgery, aftercare instructions will be given. Postoperative eye drops are given, usually as a combination of antibiotic, steroid and a non-steroidal anti-inflammatory drop as well.
There are some decisions that as a patient, you will be asked and it is worth thinking about these in advance. These include: type of anaesthetic; lens choice and whether you would like one eye at a time or both done together. There will be advantages and disadvantages to each choice and it is worth understanding these before proceeding to surgery.
This is why it is important to set your surgeon before surgery and spend some time talking through these decisions, because as outlined above, cataract surgery is ideally only performed once in your lifetime and the lens that is placed will last for your whole life.

